'Feel-good' hormone serotonin regulates blood sugar concentration
Scientists from Berlin and Maribor reveal serotonin’s role in the pancreas and its implication in diabetes
Diabetes is the most prevalent metabolic disease in developed countries and one that engenders - in addition to its high fatality - enormous health care costs. The physiological meaning of the ‘feel-good’ hormone serotonin in insulin-producing cells of the pancreas was not understood for more than 40 years but has finally been resolved by scientists of the Max Planck Institute of Molecular Genetics in Berlin. The researchers Diego J. Walther, Nils Paulmann and colleagues report in the current issue of PloS Biology, that a lack of serotonin in the pancreas causes diabetes. The interdisciplinary research team identified the underlying molecular and physiological mechanisms. The close interdisciplinary collaboration with Marjan Rupnik, head of the Institute of Physiology in Maribor, Slovenia, and a former group leader at the Max Planck Institute for Biophysical Chemistry, as well as the collaboration with Heidrun Fink, executive director of the Institute of Pharmacology and Toxicology of the School of Veterinary Medicine, Free University Berlin, was particularly instrumental to allowed untangling these findings (Paulmann et al., PloS Biology, October 27, 2009).

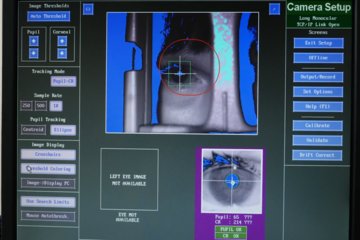
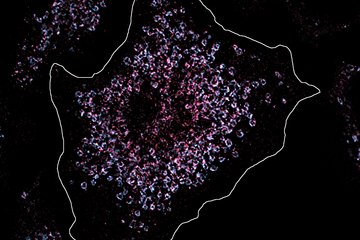
Prior studies of the team from Berlin have identified a novel mechanism of serotonin’s action in blood platelets that relies on the permanent covalent coupling of the hormone to signalling proteins, the so-called ‘serotonylation’. The scientists now identified this mechanism also in β-cells of the pancreas. As in thrombocytes, serotonylation regulates the secretion of storage granules from these cells. "Under normal conditions serotonin controls the release of insulin, the most important hormone in the regulation of blood glucose concentration of humans and animals", explains Diego Walther. When the serotonin levels are low like in serotonin-deficient mice, proper insulin secretion is hampered and blood glucose concentration rises to noxious levels after a meal, a hallmark of diabetes. The identification of the insulin-releasing action of serotonin opens new avenues for intervention in diabetes, a main research objective for further studies by the international team.
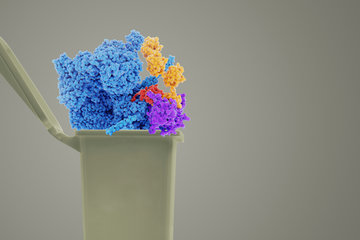
The pancreas is the third disease-associated context of serotonylation identified since the first description of this mechanism in bleeding disorders by the research team. In addition to the study’s contribution to the understanding of serotonin’s role in the widespread disease diabetes, the special case of serotonylation highlights the general physiological relevance of protein monoaminylation exemplarily. Other kinds of monoaminergic hormones like histamine, dopamine, and norepinephrine can act in similar ways. Like the phosphorylation of proteins, monoaminylation also has a profound impact on several cellular processes and their identification is a challenge accepted by the group from Berlin. Furthermore, the present study might change the text book knowledge about the mode of action of hormones. "In contrast to that which was long assumed, water-soluble hormones like serotonin, histamine, and catecholamines act not only at the cell’s interface via surface receptors, but also within cells via monoaminylation", Walther explains.
The results, published by the researchers from Berlin, solve the puzzle of what serotonin is doing in the β-cells of the pancreas and widen the concept of protein monoaminylation in disease-relevant physiological processes. The scientists plan to investigate in further studies why diabetic serotonin-deficient mice have a normal life expectancy and show none of the typical diabetes-associated secondary damage. Such research could help to improve the quality of life and to prolong life expectancy of diabetic patients.