Innate lymphoid cells regenerate within lung
Researchers generate a cell atlas of lung innate lymphoid cells
If worms infect the respiratory tract, the body reacts with a pattern that is also typical of asthma: cramping of the bronchi, elevated mucus production and a severe cough. Innate lymphoid cells (ILCs) are an essential but incompletely understood player in this worm defense. ILCs emerge during the first days after birth; however, little research has been done to date on which subgroups of ILCs exist and how they are regenerated during life. Now, Max Planck researchers from the group of Dominic Grün teamed up with a group from the University of Würzburg headed by Georg Gasteiger and generated a comprehensive atlas of lung ILCs. They made use of the powerful single-cell RNA-seq technology and identified progenitor ILCs, comprising circulating and lung-resident progenitors, which differentiate and mature within the lung. They demonstrate that during parasitic worm infections these cells adapt the identity of mature lung ILCs, independent of their origin, and thus help to maintain the population of lung-resident ILCs.

The immune system is equipped with numerous cell types that effectively fight the various pathogens, humans can encounter during their lives. T cells, for example, have a receptor through which they can specifically recognize and bind antigens. However, in recent decades, cell types with similar protective properties have been discovered that do not possess a specific antigen receptor.
Only a few years ago, scientists identified a group of lymphocytes, so-called “innate lymphoid cells” (ILCs), which are now among the most important players in the body's immune defense and make a significant contribution to the fight against pathogens. Unlike T cells, ILCs do not patrol the bloodstream, but are predominantly tissue-resident cells. ILCs reside in various tissues where they interact with many immune and non-immune cell types and contribute to immune surveillance, activation of inflammatory responses, tissue homeostasis and repair and barrier functions. They are found in the bone marrow, secondary lymphoid organs such as lymph nodes and, most prominently, in non-lymphoid tissues with mucosal barriers such as the lung or the small intestine.
Ambivalent role of ILC2 in immune defense
The size of the ILC population and the subset composition varies between organs and can undergo dynamic changes during immune challenge. Type II ILCs (ILC2s) are the dominant subtype in the lung and have been shown to play a major role in immune defense against parasitic worm infection or in wound healing. On the other hand, ILC2s also contribute to the pathology of allergic respiratory inflammation such as asthma..
As in other tissues, ILC2s in the lung expand and differentiate during the first weeks of life after which a fraction persists as tissue-resident cells during adult hood. However, ILC2s can be generated and recruited from other tissues also during adult life in normal physiology and inflammatory conditions. It was unclear whether these ILC2s have specialized functions or whether they were recruited to replenish the local pool of resident cells.
Single-cell atlas of lung innate lymphoid cells
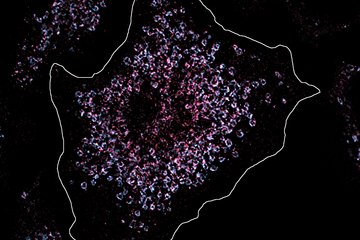
To shed light on these unknown mechanisms, scientists at the Max Planck Institute of Immunobiology and Epigenetics in Freiburg, headed by Dominic Grün, and colleagues from the Würzburg Institute of Systems Immunology led by Georg Gasteiger teamed up with researcher from New York and Marseille to generate a comprehensive single-cell atlas of mouse ILC populations in the bone marrow, neonatal and adult lung during normal physiological condition and during worm infection.
They discovered a pool of local progenitors which receives influx from the bone marrow and has the potential to generate the full spectrum of mature ILC2s observed in the lung during worm infection.
Cell plasticity in response to changing tissues
“Our work sheds light on how the local population of ILC2s in the lung is maintained. We found that progenitors recruited to the lung from other tissues via the blood stream adjust to the lung environment by modulating their gene expression and differentiate into mature ILC2s that are almost indistinguishable from their counterparts derived from lung-resident progenitors. This is an exciting example for the plasticity of immune cell states in response to changing tissue environments”, says Dominic Grün, Max Planck group leader and member of the CIBSS - Centre for Integrative Biological Signalling Studies, Cluster of Excellence at the University of Freiburg.
The study describes a “continuum” of ILC2 differentiation stages connecting the progenitors with the mature populations, including previously unknown ILC2 subtypes. “We were able to reveal the complexity of the functions of ILC2s in an unprecedented manner and at the same time draw conclusions about their origin and development,” explains Patrice Zeis, first author of the study.
To detect the heterogeneity and development of lung ILC2s in a comparable systemic way, the scientists combined single-cell RNA sequencing with machine learning approaches. Thus, they successfully created “molecular fingerprints” for thousands of innate immune cells in the murine lung, and derived novel insights on the cell’s identity, functions and the developmental relationships between the cells in the model organism. "Our proposed concepts of tissue differentiation and adaption of ILC2s may help to understand how local differentiation of ILCs can contribute to inflammatory diseases and might be applicable to other immune cell types”, explains Patrice Zeis.