Prior exposure to common cold coronaviruses enhances immune response to SARS-CoV-2
Scientists observe cross-immunity against the coronavirus
Researchers from Charité – Universitätsmedizin Berlin, the Berlin Institute of Health at Charité (BIH) and the Max Planck Institute for Molecular Genetics (MPIMG) have shown that certain immune cells, which are found in people previously exposed to common cold coronaviruses, enhance the body’s immune response to SARS-CoV-2, both during natural infection and following vaccination. The researchers, whose work has been published in Science, also report that this ‘cross-reactive immunity’ decreases with age. This phenomenon may help to explain why older people are more susceptible to severe disease and why their vaccine-induced immunity is often weaker than that of young people.

Last year, researchers from Charité and the MPIMG made a surprising discovery. They were the first to report that individuals with no prior exposure to SARS-CoV-2 nonetheless had immunological memory cells capable of recognizing this novel virus.
The researchers concluded that these ‘T helper cells’ must have been generated to deal with mostly harmless common cold coronaviruses and that, thanks to the structural similarities between coronaviruses (in particular the characteristic spike protein found on their outer surface), these T helper cells will also attack the novel coronavirus. This ‘cross reactivity’ hypothesis has since been confirmed by a range of studies.
Protective action by cross-reacting T helper cells
Still unclear, however – and the object of intense debate – is the question of whether these immune cells affect the course of subsequent SARS-CoV-2 infections. “Our assumption at the time was that cross-reactive T helper cells have a protective effect, and that prior exposure to endemic (i.e. long-established and widely circulating) coronaviruses therefore reduces the severity of COVID-19 symptoms,” says the study’s (and the previous study’s) first author, Dr. Lucie Loyal, a researcher based at both the Si-M (‘Der Simulierte Mensch – literally ‘The Simulated Human’, a joint research space of Charité and Technische Universität Berlin) and the BIH Center for Regenerative Therapies (BCRT).
She adds: “However, the opposite could have been true. With some viruses, a second infection involving a similar strain can lead to a misdirected immune response and a negative impact on clinical course.” In the current study, the Berlin-based research team presents evidence to support their previous assumptions regarding the existence of a protective effect. According to their data, cross-reactive immunity could be one of several reasons for the variability in disease severity seen with COVID-19 but might also explain differences in vaccine efficacy seen in different age groups.
A universal memory for coronaviruses
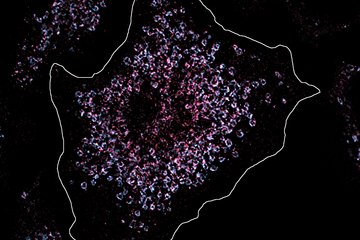
For the current study, the researchers recruited individuals with no prior exposure to SARS-CoV-2, testing them at regular intervals to establish whether they had contracted the infection. Out of a total of nearly 800 participants who were recruited from mid-2020 onwards, 17 persons tested positive. The researchers studied the affected individuals’ immune systems in detail. Their analyses showed that the immune response against SARS-CoV-2 also included the mobilization of T helper cells which had been generated in response to endemic common cold viruses.
The researchers also showed that the quality of the immune response against SARS-CoV-2 was linked to the quantity of cross-reactive cells which had been present in the body prior to infection. These cells were particularly effective at recognizing a certain area of the spike protein. In both the endemic viruses and the new coronavirus, this site was characterized by sequence similarities which were particularly well ‘preserved’.
“During infections with the more harmless coronaviruses, the immune system builds up a kind of protective ‘universal coronavirus’ memory,” explains the study’s corresponding author, Dr. Claudia Giesecke-Thiel, Head of the Flow Cytometry Service Group at the MPIMG. “Once exposed to SARS-CoV-2, these memory cells are reactivated and kick-start the response against the new pathogen. This could help accelerate the initial immune response to SARS-CoV-2 and limit viral propagation during the early stages of the infection and is therefore likely to have a positive effect on the course of the disease.”
Taking a more cautionary tone, the researcher adds: “This does not mean that prior exposure to common cold viruses will definitely protect an individual against SARS-CoV-2, nor does it change the course of the pandemic as of now because these underlying mechanisms have been operating all along. It in no way diminishes the importance of getting vaccinated. Our study provides one of several explanations for an observation made since the beginning of the pandemic, namely that the symptoms of SARS-CoV-2 infection can vary greatly between individuals.”
Immune-boosting effect also for vaccination
The researchers’ findings furthermore confirmed that the immunity-enhancing effects of cross-reactive T cells also occur following vaccination with the BioNTech COVID-19 vaccine. Just like natural infection, the vaccine prompts the body to produce the SARS-CoV-2 spike protein (including the well-preserved section of it) and present it to the immune system.
An analysis of the immune responses of 31 healthy individuals before and after vaccination revealed that, while the activation of normal T helper cells took place gradually over the course of two weeks, the activation of cross-reactive T helper cells was extremely rapid, taking place within one week of vaccination. Naturally, this also had a positive effect on the generation of antibodies. Even after the first dose of the vaccine, the body was able to produce antibodies against the preserved section of the spike protein at a rate normally only seen after booster vaccinations.
“Even following vaccination, the body is able to utilize at least some of its immunological memory – provided it has had previous exposure to endemic coronaviruses,” says co-corresponding author Prof. Dr. Andreas Thiel, a Charité researcher based at both the Si-M and the BCRT. He adds: “This might explain the surprisingly rapid and extremely strong protective effect we see after the initial dose of the COVID-19 vaccine, at least in younger individuals.”
Decline with age
In a second part of the study, the researchers analyzed T helper cells in approximately 570 healthy individuals. They were able to show that cross-reactive immunity declines in older adults. In fact, both the number of cross-reactive T cells and the strength of their binding interactions was shown to be lower in older participants than in younger participants. According to the authors, this decline in cross-reactive immunity is caused by normal, age-related changes. “Infection with an endemic coronavirus represents a benefit in younger people, helping them fight off SARS-CoV-2 or develop immunity following vaccination. Sadly, this benefit is less pronounced in older adults,” says Prof. Thiel. He adds: “It is likely that a third (or booster) dose would be able to compensate for this weaker immune response, ensuring that members of this high-risk group have adequate immunity.”