Thymic cancer
Researchers clarify the origin of a rare disease
The thymus is crucial for the defense against infectious diseases as well as cancer. In rare cases, a tumor can develop in this inconspicuous organ, and little is known about the development of thymic cancer. Researchers at the Max Planck Institute of Immunobiology and Epigenetics in Freiburg have now developed the first animal model to track down the origin of thymic cancer. The results show that the tumor arises from cells whose maturation is blocked by certain genetic alterations, thereby weakening the immune defense.

The thymus located in the thorax is essential for our immune defense. In this organ, various types of T cells mature, including the famous killer cells, which can specifically destroy virus-infected and malignant cells, and so-called T helper cells, which support antibody-producing B cells in fighting foreign substances in the body. The thymus develops its most significant activity during the first years of life, as the body’s immune system must be quickly and reliably equipped with effective defense cells. After fulfilling this essential task, the thymus becomes smaller. However, even in advanced age, the thymus does not disappear completely.
In rare cases, malignant degeneration of the thymic tissue occurs. Even though the majority of these tumors grow slowly, they require rapid treatment to save the patient’s life. Surgical removal is the mainstay of therapy since the origin and characteristics of thymic tumors are poorly understood. Only a better understanding of these conditions enables the development of targeted therapies.
Effects of a mutated gene switch identified
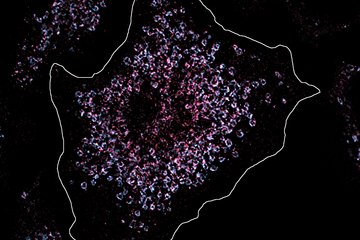
A well-established and successful approach in cancer research is the use of animal models to study the characteristics of different types of cancer and to test novel forms of therapy. Researchers led by Prof. Thomas Boehm at the Max Planck Institute of Immunobiology and Epigenetics in Freiburg took this approach. Their starting point was the discovery of a genetic alteration in a gene that often occurs in thymic tumors and acts as a switch for the activation of numerous other genes. However, it was previously unclear how this inconspicuous variation in the gene called GTF2I leads to tumorigenesis. The researchers used a molecular trick to answer this question. They altered the genetic information of mice in such a way that the affected animals activate the mutated switch in the thymus. From the comparison with healthy mice, the changes in the thymus of the diseased animals could be precisely tracked.
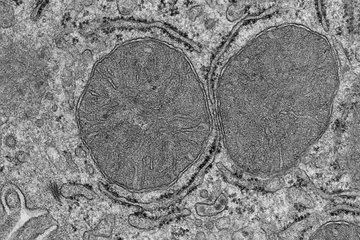
There are two classes of cells in the thymus. The first type, called stroma, provides a niche in which the second type of cells, the already mentioned immune cells, settle and mature until they can leave the thymus and perform the surveillance function in the body. The genetic alteration in the GTF2I gene found in tumors affects the stromal cells, which are renewed throughout life from so-called stem cells. The study shows that the mutated GTF2I gene inhibits the renewal of stromal cells. As a result, they stop halfway and can, therefore, only insufficiently perform their support function for maturing immune cells. This effect becomes more noticeable with advancing age and may explain the accumulation of thymic cancer in the second half of life.
This discovery is significant in two respects. On the one hand, the team in Freiburg was able to identify a previously unknown intermediate step in the formation process of the stroma in the thymus. And on the other hand, they could show that this marks a particular susceptibility to malignant transformation of the thymus organ. Moreover, the studies show how drugs can be specifically tested to see whether they can break through this blockage and thus normalize the formation of the stroma again. “Our study shows again how important animal experiments can be for progress in understanding human tumor diseases. This is particularly true for rare diseases such as thymic cancer, which often receive only little attention,” says Thomas Boehm.
The researchers now want to refine their animal model to make it even more similar to the situation found in patients. In particular, they hope that a precise understanding of the gradual development of the tumors will enable them to develop a stage-dependent therapy concept that could allow risk-adapted treatment of the patients affected.