Lupus trigger discovered
Researchers were able to trace a form of the autoimmune disease lupus back to a single mutation
Sometimes a single mutation in our genetic make-up is enough to cause disease. This is also the case with the autoimmune disease lupus. Lupus causes severe inflammation throughout the body and can have a serious impact on the lives of those affected. Researchers at the Max Planck Institute for Infection Biology in Berlin have now discovered a mechanism that can trigger lupus in children. This mechanism regulates the amount of a specific immune receptor that normally recognizes the genetic material of pathogens. If this mechanism is disrupted, receptors accumulate in the immune cells leading to the recognition of the body's own genetic material. As a result, the immune system turns against its own body and causes the systemic inflammation of lupus. In collaboration with physicians from the Hospital of the Ludwig Maximilian University of Munich, the researchers were able to identify a lupus patient in whom this mechanism is disrupted by a single mutation.

The innate immune system responds to invading pathogens within minutes. It is an initial line of defence that keeps pathogens at bay until the more specific adaptive immune system kicks in. However, this speed comes at a price: the innate immune system’s response is so strong and unspecific that it must be well controlled to prevent it from turning against the body itself.
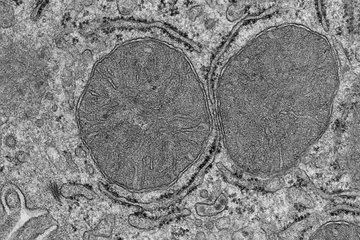
In Olivia Majer’s group at the Max Planck Institute for Infection Biology, researchers are working to better understand these control mechanisms of the innate immune system. The group is focusing on an immune receptor called Toll-like receptor 7, which can recognize the genetic material of viruses and bacteria and then triggers an immune response against the invaders.
Immune receptor out of balance
In order for the immune system to react quickly, a certain number of these receptors must be present in the immune cells. Cells maintain this balance by constantly producing and degrading receptors. “We wanted to understand what happens when this balance is disturbed,” explains group leader Olivia Majer.
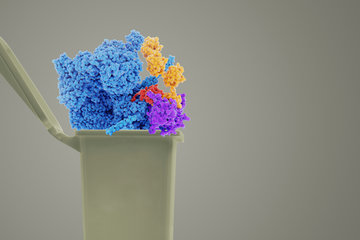
During their work, Majers’ team became interested in a protein complex called BORC. The researchers were able to show that BORC is required to degrade Toll-like receptor 7 within the cell. In addition, BORC needs another protein, UNC93B1, to carry out the degradation process correctly. If there is an error in this process, the receptor is not degraded and accumulates in the immune cells. “From earlier experiments in mice carried out a few years ago at the University of Berkeley in California, we already knew that too many of these receptors are a problem,” explains Majer. A greater amount of receptor biases towards recognizing the body’s own genetic material. This leads to an immune response against self, a trigger for the autoimmune disease lupus. So far, however, neither BORC nor UNC93B1 have been associated with lupus in humans.
The researchers received confirmation of their findings by phone. Fabian Hauck teaches, researches and treats patients at the Ludwig Maximilian University Hospital in Munich, and specialises in congenital immune disorders such as lupus. He became aware of Majer's research because one of his patients had a mutation in the gene for a previously unnoticed protein: UNC93B1. It was precisely this protein that Majer had identified with her team. “When I got the first call from Fabian Hauck, I thought it was too good to be true,” says Majer, “but within eight busy weeks of joined effort, we were able to confirm that the mutation in UNC93B1 was the cause of this patient’s lupus.”
A new approach for lupus therapies
Hauck and Majer’s findings have now been published in the prestigious journal Science Immunology. At the same time, the journal also published the work of a research group at the Technical University of Dresden, with whom the two researchers collaborate. In their study, the Dresden scientists identified additional UNC93B1 mutations that can trigger lupus. The researchers have uncovered a completely new mechanism that triggers a particularly aggressive form of lupus: severe symptoms develop as early as infancy, while many other forms of lupus only appear in adults.
Testing for mutations in UNC93B1 could quickly become part of lupus treatment, opening up new approaches to therapy. In the past, doctors have mainly focussed on suppressing inflammation with drugs. By targeting the mechanism that has now been discovered, it may be possible to prevent the inflammation from developing in the first place—and thus significantly reduce the disease burden for those affected.