Growth treatments for nerve cells
A damaged nerve in a finger will heal, but a damaged nerve in the brain or spinal cord will not. Frank Bradke and his research group at the Max Planck Institute of Neurobiology in Martinsried want to encourage nerve cells in the spinal cord to regrow after injury.
Text: Frank Bradke and Stefanie Merker

I have always been impressed by the body’s ability to heal itself. A cut on your finger destroys skin cells, injures muscles and blood vessels and severs nerve cell extensions. It is painful, but not a catastrophe. After a short time, nerve cells regrow, muscles and blood vessels are reconstructed and the skin closes over the cut.
Even more serious injuries usually heal without leaving significant traces, although the cells occasionally have to be persuaded to grow in the right direction with a bandage or a splint. But what’s wrong with this picture? If the body has these astonishing self-healing powers at its disposal, why doesn’t it use them to repair its most delicate systems, the brain and the spinal cord?
The nervous system is divided into two areas: the brain and the spinal cord form the central nervous system, while all other nerves, such as those in the arms and legs, make up the peripheral nervous system. One important difference between these two systems lies in their ability to regenerate. Unlike those in the peripheral nervous system, the cells in the central nervous system hardly ever recover from damage.
Depending on where in the brain the injured cells are located, many different impairments can result, most of which are permanent. Accidents involving head injuries, diseases such as multiple sclerosis or Parkinson’s, and strokes are frequent causes of cell death in the brain.
When nerves in the spinal cord are badly crushed or severed, lifelong paralysis can result. The closer to the neck the injury occurs, the more severe the paralysis. A study in the US showed that, in that country alone, there are 8,000 to 11,000 cases annually of spinal cord injuries that result in paralysis. In 47 percent of these patients, the legs are paralyzed, and in 52 percent, both the arms and the legs. Accidents are often the cause of injury to the spinal cord, which is why paralysis is frequent in 16- to 30-year-olds. As those affected have a relatively normal life expectancy, their number increases globally from year to year.
Stop Signs in the neural network
With so many people impacted in this way, an urgent search is underway for an answer to why nerve cells in the central nervous system do not regrow their extensions after an injury. For me and many of my colleagues, this is one of the most fascinating questions in modern neurobiology. In the past 10 to 15 years, intensive basic research has brought about considerable progress in this area. For example, a number of factors have been found in the nerve cell environment that can stop the nerve cell extensions from growing.

These factors can be imagined as stop signs: as a responsible road user, a cell extension stops growing when it reaches one of these stop signs. And this is precisely the problem: as soon as the nervous system is fully developed, these stop signs are put up throughout the central area. When the nerve cell extensions in an adult organism are severed, they are faced with a forest of stop signs. As long as these signs are present, the cell extensions can grow no further. This also means that once contact with partner cells has been broken off, it cannot be re-established. The consequence is paralysis.
But what would happen if the nerve cells could be turned into more daring road users that would simply ignore the signs and grow right past them, more or less the way it is in everyday traffic situations? This question has not only occupied my thoughts while driving, it is also the main subject of my work at the Max Planck Institute of Neurobiology. This is where my research group and I are examining the mechanisms inside the cells that are responsible for stopping cell growth in the central nervous system. We have set out to look for the brake, so to speak, that brings the cells to a halt in front of the stop signs. We are hoping that we will be able to release this brake for long periods, or even deactivate it completely.
What actually happens in the extension of a central nervous system cell when it stops growing after an injury? It could be assumed that these nerve cells are unable to regrow at all after an injury. Fortunately, though, there are nerve cells whose extensions project into both the central and the peripheral nervous systems. If these cells are damaged in the peripheral section, they regrow after a short time – as in our example with the cut finger.
An insider’s view of the growth cone
When an injury occurs in the central nervous system, the damaged extensions of the cells do not regrow. However, when the same cell is damaged first in the peripheral section and then in the central section, it will also be able to regrow in the central nervous system. These observations show that nerve cells in the central nervous system can, in principle, recover from an injury.

In order to understand why the cells nevertheless do not grow after being damaged, it is helpful to recall the structure of nerve cells and how they develop. A typical nerve cell consists of a cell body and a series of extensions. Depending on the cell type, they can develop into axons and/or dendrites. Like a long cable, an axon propagates incoming information to remote nerve cells; dendrites collect information from many different nerve cells with their fine branches. The separate pieces of information coming from the dendrites are computed and the result passed on to other cells via an axon. It is often the long axons that are severed when injuries occur, which means that the growth of these connecting cables is particularly significant.
At the tip of a growing axon, for instance from a young nerve cell, there is a growth cone where, quite literally, everything goes on. This is home to special proteins that allow the axon to find its way to the correct partner cell among thousands of nerve cells.
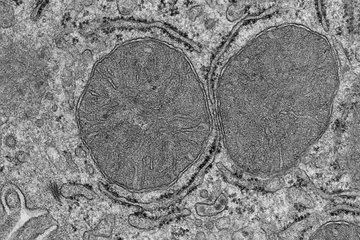
In addition, the growth cone contains many mitochondria, the cellular powerhouses, and parallel bundles of microtubules without which the axon could not extend. Microtubules are tiny protein tubes that lengthen the axon by means of a coordinated push forward. Thus, in our search for the brake in the cell, the microtubules seemed to be a very promising place to start our research. Perhaps it would be possible to use the microtubules to make a damaged axon grow past the stop signs.
When an axon in the peripheral nervous system is severed, a growth cone forms at its tip – exactly in the same way as in a young cell – and the axon grows anew. The tip of a damaged axon in the central nervous system also thickens. However, unlike the growth cone, this axonal bulb shows no inclination to grow. On the contrary: we observed that, in the weeks following the injury, the axonal retraction bulb continued to swell, but stopped moving forward to extend the axon for an indefinite period.
Taxol stabilizes microtubuli
What happens in this retraction bulb, and what prevents the axon from continuing to grow? These questions are key to understanding the growth brake in the central nervous system. For a long time, it was impossible to directly observe how the retraction bulb formed. Our research group was one of the first to attempt to get to the bottom of these fascinating questions. This was possible thanks to the great progress made in genetics in recent years, which has brought increasing numbers of new methods and analyses. For example, it recently became possible to mark individual nerve cells with green fluorescent protein (GFP).

This has revolutionized neurobiology: scientists are no longer faced with a confusing array of thousands of identical nerve cells, but can precisely mark individual cells or cell components and study them. The discovery of GFP was also fortuitous for my work, as it enabled us to visualize what was happening in the retraction bulb.
My colleague Ali Ertürk discovered that a retraction bulb can be identified less than an hour after an injury. While it slowly swells during the ensuing hours, mitochondria accumulate inside it, which is similar to what happens in a growth cone. With these cellular powerhouses on the job, it is rather unlikely that the growth stop is caused by a lack of energy. Things became really interesting, however, when we looked at the microtubules. Normally they are in a very regular parallel arrangement, like a set of railroad tracks; in the retraction bulb, however, they were completely jumbled. No wonder they weren’t making any headway!
But is it really the disarranged microtubules that prevent the axon from continuing to grow? We used a substance called nocodazole to test this. Nocodazole is frequently used in cell biology to destabilize microtubules. And indeed, when we added nocodazole to growth cones, they became retraction bulbs, and the axons ceased to grow. This was proof that the disordered microtubules in the bulb are one of the main reasons why the axon stops growing. This result was quickly followed by the next question. What if we replaced the nocodazole with a substance that would stabilize the microtubules?
Taxol suggested itself for these investigations. In cancer therapy, the microtubule stabilizing action of Taxol stops cancer cells from dividing. In our experiments, Taxol exhibited similarly encouraging effects: My colleague Harald Witte was able to help a young cell decide which of its extensions should become an axon. The addition of Taxol stabilized the microtubules of any randomly chosen extension and allowed it to grow into an axon.
A barrier of scar tissue
Untreated extensions developed into dendrites. When we injected Taxol directly into a CNS lesion in the living organism, the formation of retraction bulbs was suppressed and the cut axon did not retract from the lesion. Furthermore, my colleague Farida Hellal showed in cell culture experiments that Taxol enables damaged nerve cells in the central nervous system to grow again, even when we surrounded the nerve cells with “stop sign” molecules.

The results of these studies are quite encouraging. In a relatively short time, we have found out a great deal about what happens in the axonal retraction bulb. We also now know one of the reasons why damaged axons in the central nervous system do not continue to grow. The next steps are to find out whether Taxol works in the same way in living organisms. We also need to find the correct dosage and a way of administering it. Too much Taxol suppresses the dynamics of the microtubules so that axons cannot grow properly. These problems need to be resolved, first in the laboratory and then in clinical studies.
However, I believe that, in the long term, microtubule stabilization is a promising approach to improving regeneration of axons in the central nervous system. Nevertheless, there are still many open questions, and it will take years before medicine will be able to heal paraplegia. The impact of other factors, such as nerve scar tissue, is still unknown. This nerve tissue initially protects the cells from further injury, but it also forms a barrier that prevents the regrowth of the cells. How to reduce this scar tissue and how to make the nerve cells not only ignore the growth stop signs but also break through the scar barrier are some of the questions we will be looking at next.