Assembly within the tumor center
Number of macrophages in tumor tissue enables prognosis of lung tumor progression

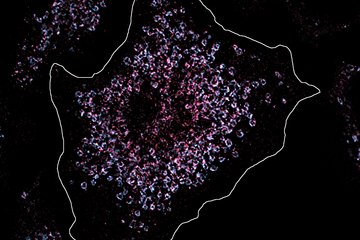
Tumor cells and two different macrophage populations visualised by means of multiplex immunofluorescence microscopy (left) were subjected to a complex location analysis (right scheme). The scheme shows tumor cells in green, tumou-inhibiting macrophages in blue and tumor-promoting macrophages in red.
Immune cells significantly influence the course of tumors. Depending on the cell type, they can both promote and inhibit tumor growth. This is particularly true for a group of macrophages, which accumulate in the tumor center or the peripheral areas in sometimes large numbers. Depending on their activation state, these so-called tumor-associated macrophages can have a positive or negative influence on the course of the disease.
Scientists at the Max Planck Institute for Heart and Lung Research and the Justus Liebig University in Giessen discovered that the accumulation of a subpopulation of tumor-associated macrophages in a certain area can lead to conclusions about the further course of the tumor disease. Rajkumar Savai, project leader in the department "Development and Remodelling of the Lung" and member of the Centre for Internal Medicine at Justus Liebig University explains: "With lung tumors, it is usually possible to distinguish the center of the tumor from the peripheral area. Because a particularly large number of immune cells migrate to the latter, we refer to this area as the invasive tumor margin".
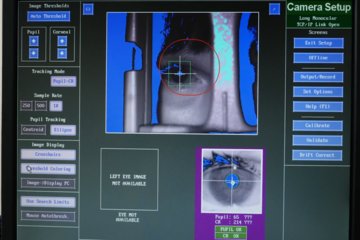
For their study, the researchers used an elaborated microscopy technique known as multiplex immunofluorescence microscopy. By this technique, macrophages could be safely identified. Furthermore their distance from neighbouring tumour cells was analysed. In addition, the Max Planck researchers divided these cells into tumor-promoting and tumor-inhibiting tumor-associated macrophages based on certain properties. "We found that more tumor-promoting cells were found in the invasive border area of the tumor than tumor-inhibiting cells. Moreover, they were located more adjacent to the tumor cells," said Savai. "Based on tissue samples from more than a hundred patients, we were then able to identify a pattern."
According to this study, the survival rate in lung cancer patients was lower, in particular when the tumor-promoting macrophages in the invasive marginal areas were particularly close to the tumor cells and at the same time tumor-inhibiting macrophages were further away. The cell number also had an influence on the prognosis of the patients: "If there were fewer tumor-inhibiting macrophages in the tumor center, patients had a lower probability for surviving. Overall, we found more tumor-promoting macrophages than tumor-inhibiting macrophages," Savai said.
The fact that tumor-promoting and tumor-inhibiting macrophages actually have different activity patterns was shown when the Bad Nauheim scientists sequenced the cells' RNA. "We found that the two cell variants had very different gene expression profiles, even when compared with macrophages from outside the tumor tissue," said Savai. The researchers identified five candidates for biomarkers that could be used to predict survival in lung cancer. "These biomarkers could prove to be very helpful for the individual treatment strategy of lung cancer patients," emphasizes Friedrich Grimminger, head of the Giessen Lung Tumor Center and director of the Medical Clinic IV/V at Justus Liebig University. "Based on characteristic gene expression profiles of the tumor-associated macrophages, we have also identified factors in this study that offer themselves as new target structures for specific therapeutic approaches," adds Werner Seeger, Director of the Department "Development and Reconstruction of the Lung" at the Max Planck Institute and the Medical Clinic II of Justus Liebig University.
MH