Bacteria poison themselves from within
Potential new antibiotics use a bacterial suicide mechanism
The research group led by Anton Meinhart at the Max Planck Institute for Medical Research in Heidelberg has shown that proteins from the zeta toxin group trigger a self-destructive mechanism in bacteria. The triggers for this bacterial suicide are toxin/antitoxin systems that play an important role in the hereditary transmission of resistance and virulence genes. The scientists have thus found a valuable new tool for the development of new broad-spectrum antibiotics.

A small number of genes can make dangerous killers out of innocuous bacteria. Genes that carry pathogenic properties or resistance to antibiotics can be transmitted from bacterium to bacterium by means of so-called mobile genetic elements. However, these elements often also contain genes for toxins and the corresponding antitoxins. “The mobile genetic elements are a two-edged sword to the bacteria: they help them survive, but can also kill them”, says Anton Meinhart from the Heidelberg institute.
The PezAT (pneumococcal epsilon zeta antitoxin toxin) system is a particularly interesting toxin/antitoxin system of the pathogen Streptococcus pneumoniae. These bacteria, which are also termed pneumococci, cause serious infections such as pneumonia, septicaemia and meningitis. The toxin component PezT belongs to the family of zeta toxins; these are known to stabilise mobile genetic elements which transmit resistance in many other pathogens. Although the zeta toxin family was discovered almost 20 years ago, its deadly mechanism had remained a mystery until now. The toxins seemed to attack a very early cellular process since, besides bacteria, they are able to kill off both yeast and cancer cells.

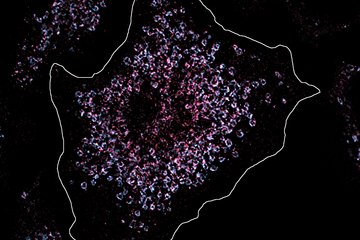
However, the Max Planck scientists have now managed to explain the molecular mode of action of zeta toxins using the model bacterium Escherichia coli. As it turned out, bacterial cells in which PezT was activated artificially showed symptoms of poisoning similar to those occurring after treatment with the well-known antibiotic penicillin: at the beginning of the PezT poisoning, most of the cells stalled in the middle of their division stage. After a period of time, the intersection between the two cell bodies burst and the cells died.
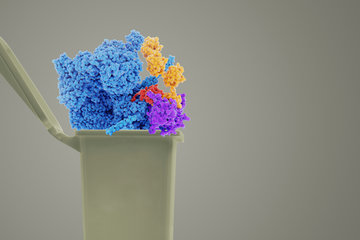
After further investigation, the scientists found that PezT and other zeta toxins are novel enzymes that transform the essential sugar building block UNAG (UDP-N-acetylglucosamine) into a toxic molecule. The toxin (UNAG-3P), very much like penicillin, inhibits the growth of the bacterial cell wall, causing the cells to burst and die. This process of internal cell activation could bring research on antibiotics a major step forward in the battle against bacterial resistance.
The zeta toxins are the first known enzymes known to poison bacteria from within by producing a ’suicide antibiotic‘. Since the building block UNAG is responsible for the growth of the cell wall in all known bacteria, this discovery explains the broad effectiveness of zeta toxins, or more specifically, UNAG-3P. It also makes the newly discovered substance UNAG-3P a valuable basic material for the development of innovative broad-spectrum antibiotics. In a next step, the scientists therefore want to determine whether UNAG-3P can be used as a new effective antibiotic.
Moreover, their discovery enabled the scientists to explain a hitherto paradoxical phenomenon: namely, that the supposedly lethal pneumococcal zeta toxin PezT boosts the pneumococcal infection rate. The reason for this is probably that an activation of PezT causes the bacterium to burst, and thereby releases its constituents. In this process, one of the most important pneumococcal toxins, pneumolysin, can spread and cause severe inflammation. It therefore seems that individual pneumococci sacrifice themselves for the good of the total population in the battle against the immune system.
AM/HR
Background
The toxin/antitoxin system
Most bacteria that colonise our environment pose no threat to us humans. However, a small number of additional bacterial genes are sufficient to transform an innocuous unicellular organism into a dangerous pathogen that is resistant to antibiotics
The majority of these “virulence factors” are transmitted from one bacterium to the next by so-called mobile genetic elements. This exchange of genes can take place even between species that, from an evolutionary point of view, are very far removed from one another, and is one of the main reasons for the rampant appearance of new multi-resistant germs.
Nevertheless, to gain these new advantages, the bacteria must often sign a pact with the devil. Because the mobile genetic elements are unstable and constantly risk being eliminated from the bacterial genome, e.g., during cell division, they contain toxin/antitoxin systems in addition to the virulence and resistance genes. These small DNA sections consist of only two genes that generate a fatal addiction. Once they are part of the bacterial genetic makeup, the bacterium starts to produce the two gene products of a toxin/antitoxin system: a strong toxic protein (‘toxin’) which threatens to poison the cell from within, and an ‘antitoxin’ which neutralises the toxin by interacting with it. While the antitoxin is present, the bacterium can initially continue to exist little affected by receiving a toxin/antitoxin system. However, the antitoxin molecules are perfidiously eliminated faster through the cellular degradation mechanisms than the toxin. The cells must therefore continue to synthesise the antitoxin in order to avoid poisoning by the toxin. If a cell loses the mobile genetic element with the toxin/antitoxin system, the production of the antitoxin is blocked. This causes the toxin to be released and leads to a ’programmed‘ bacterial cell death. The only cells able to survive are those possessing the mobile genetic elements containing the toxin/antitoxin system.
Thanks to this selection mechanism, the mobile genetic elements can avoid disappearing from the genetic makeup, even if the bacteria are not threatened by antibiotics. Even in the absence of the selection pressure exerted by antibiotics, they are maintained – together with any resistance genes – although they represent a potential threat to the cells. Toxin/antitoxin systems therefore have the potential to kill off bacteria, but could also be responsible for the stabilisation of resistance. Further study of these will be important in future research on antibiotics.
Recent evidence increasingly suggests that toxin/antitoxin systems have other selective advantages and have taken on further functions in the course of bacterial evolution. For instance, if a bacterial population is in danger of disappearing due to starvation, certain TA systems seem to provoke an ’altruistic‘ death of a subpopulation, in order to release nutrients and ensure the survival of the main bacterial population.